14129871
ANA - Heart failure care
Resumen del Recurso
Pregunta 1
Pregunta
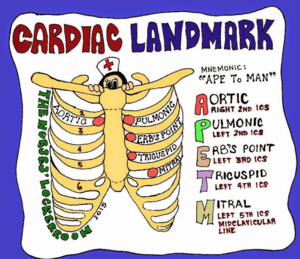
Heart failure impacts quality of life and interferes with activities of [blank_start]daily living[blank_end]. Reducing myocardial [blank_start]oxygen[blank_end] demand is a major nursing care [blank_start]goal[blank_end] for the individual in acute [blank_start]heart failure[blank_end]. This includes providing [blank_start]rest[blank_end] and undertaking the prescribed interventions to reduce cardiac work, improve contractility and manage [blank_start]symptoms[blank_end]. See also the accompanying nursing care plan for additional nursing diagnoses and interventions for the individual with heart failure. ■ [blank_start]Auscultate[blank_end] the person’s heart and breath sounds regularly. [blank_start]S1[blank_end] and [blank_start]S2[blank_end] may be diminished if cardiac function is poor. A ventricular [blank_start]gallop[blank_end] (S3) is an early sign of heart failure; atrial gallop ([blank_start]S4[blank_end]) may also be present. [blank_start]Crackles[blank_end] are often heard in the lung bases; increasing [blank_start]crackles[blank_end] and [blank_start]dyspnoea[blank_end] indicate worsening failure.
Lemone, Priscilla. Medical-Surgical Nursing (Australian Edition) Volumes 1-3 (Page 1053). P.Ed Australia. Kindle Edition.
Respuesta
-
daily living
-
oxygen
-
goal
-
heart failure
-
rest
-
symptoms
-
Auscultate
-
S1
-
S2
-
gallop
-
S4
-
Crackles
-
crackles
-
dyspnoea
Pregunta 2
Pregunta
Decreased cardiac [blank_start]output[blank_end] Pump failure results in decreased upstroke [blank_start]volume[blank_end] and tissue [blank_start]perfusion[blank_end]. ■ Monitor the person’s vital signs and oxygen [blank_start]saturation as[blank_end] indicated. Decreased cardiac output stimulates the SNS to [blank_start]increase the heart rate[blank_end] in an attempt to restore CO. [blank_start]Tachycardia[blank_end] at rest is common. [blank_start]Diastolic[blank_end] blood pressure may initially be elevated because of [blank_start]vasoconstriction[blank_end]; in late stages, compensatory mechanisms fail and the person’s BP will [blank_start]fall[blank_end]. Oxygen saturation levels provide a measure of [blank_start]gas exchange[blank_end] and tissue [blank_start]perfusion[blank_end]. CONSIDERATION FOR PRACTICE Report manifestations of decreased [blank_start]cardiac output[blank_end] and tissue perfusion including changes in mentation, decreased [blank_start]urine[blank_end] output, cool, clammy skin, diminished pulses, pallor or [blank_start]cyanosis[blank_end], and arrhythmias.
Lemone, Priscilla. Medical-Surgical Nursing (Australian Edition) Volumes 1-3 (Page 1053). P.Ed Australia. Kindle Edition.
Respuesta
-
output
-
volume
-
perfusion
-
saturation as
-
increase the heart rate
-
Tachycardia
-
Diastolic
-
vasoconstriction
-
fall
-
gas exchange
-
perfusion
-
cardiac output
-
urine
-
cyanosis
Pregunta 3
Pregunta
Administer supplemental [blank_start]oxygen[blank_end] as needed. This improves oxygenation of the [blank_start]blood[blank_end], decreasing the effects of [blank_start]hypoxia[blank_end] and ischaemia. ■ Administer prescribed medications as ordered. Drugs are used to decrease the [blank_start]cardiac workload[blank_end] and increase [blank_start]contractility[blank_end]. ■ Encourage rest, explaining the rationale. [blank_start]Elevate[blank_end] the head of the bed to reduce the [blank_start]work of breathing[blank_end]. Provide a bedside commode and assist with activities of daily living (ADLs). Instruct the person to avoid the Valsalva manoeuvre and encourage the use of stool softeners to reduce strain. These measures reduce cardiac workload.
Lemone, Priscilla. Medical-Surgical Nursing (Australian Edition) Volumes 1-3 (Page 1053). P.Ed Australia. Kindle Edition.
Respuesta
-
oxygen
-
blood
-
hypoxia
-
cardiac workload
-
contractility
-
Elevate
-
work of breathing
Pregunta 4
Pregunta
Excess [blank_start]fluid volume[blank_end] As cardiac output [blank_start]falls[blank_end], compensatory mechanisms cause salt and water [blank_start]retention[blank_end], increasing [blank_start]blood volume[blank_end]. This increased fluid volume places additional [blank_start]stress[blank_end] on the already failing [blank_start]ventricles[blank_end], making them work harder to move the fluid load. ■ Assess [blank_start]respiratory[blank_end] status and auscultate lung sounds at least every [blank_start]4[blank_end] hours. Notify the doctor of [blank_start]significant changes[blank_end] in condition. [blank_start]Declining[blank_end] respiratory status indicates worsening [blank_start]left[blank_end] heart failure.
Lemone, Priscilla. Medical-Surgical Nursing (Australian Edition) Volumes 1-3 (Page 1053). P.Ed Australia. Kindle Edition.
Respuesta
-
fluid volume
-
falls
-
retention
-
blood volume
-
stress
-
ventricles
-
respiratory
-
4
-
significant changes
-
Declining
-
left
Pregunta 5
Pregunta
■ Monitor the person’s [blank_start]intake and output[blank_end]. Notify the doctor if urine output is less than [blank_start]30[blank_end] mL/h. [blank_start]Weigh[blank_end] daily. Careful monitoring of [blank_start]fluid volume[blank_end] is important during treatment of heart failure. [blank_start]Diuretics[blank_end] may reduce circulating volume, producing hypovolaemia despite persistent peripheral oedema. A fall in urine output may indicate significantly [blank_start]reduced[blank_end] cardiac output and renal [blank_start]ischaemia[blank_end]. Weight is an [blank_start]objective[blank_end] measure of fluid status: 1 L of fluid is equal to [blank_start]1[blank_end] kg of weight. ■ Record their abdominal [blank_start]girth[blank_end] every shift. Note complaints of a loss of [blank_start]appetite[blank_end], abdominal [blank_start]discomfort[blank_end] or nausea. Venous congestion can lead to ascites and may affect [blank_start]gastrointestinal[blank_end] function and nutritional status. ■ Monitor and record the person’s haemodynamic measurements. Report significant changes and negative trends. Haemodynamic measurements provide a means of monitoring condition and response to treatment. ■ Restrict fluids as [blank_start]ordered[blank_end]. Offer appropriate choices of fluid type and timing of intake, scheduling most fluid intake during [blank_start]morning[blank_end] and [blank_start]afternoon[blank_end] hours. Offer ice chips and frequent [blank_start]mouth care[blank_end]. Providing choices increases the person’s sense of control. Ice chips and frequent mouth care relieve [blank_start]dry mouth[blank_end] and thirst and promote comfort.
Lemone, Priscilla. Medical-Surgical Nursing (Australian Edition) Volumes 1-3 (Page 1054). P.Ed Australia. Kindle Edition.
Respuesta
-
intake and output
-
30
-
Weigh
-
fluid volume
-
Diuretics
-
objective
-
reduced
-
ischaemia
-
1
-
girth
-
appetite
-
discomfort
-
gastrointestinal
-
ordered
-
morning
-
afternoon
-
mouth care
-
dry mouth
¿Quieres crear tus propios Tests gratis con GoConqr? Más información.